100% Telehealth, defined
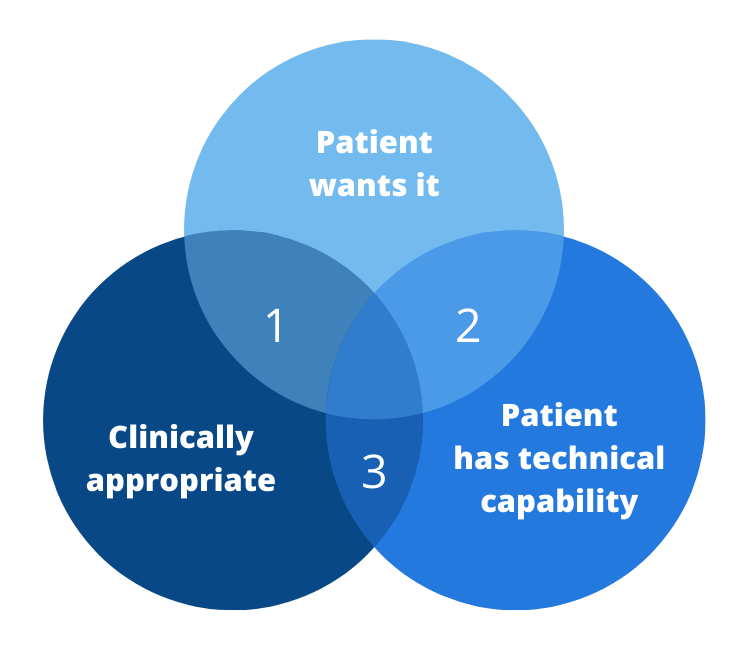
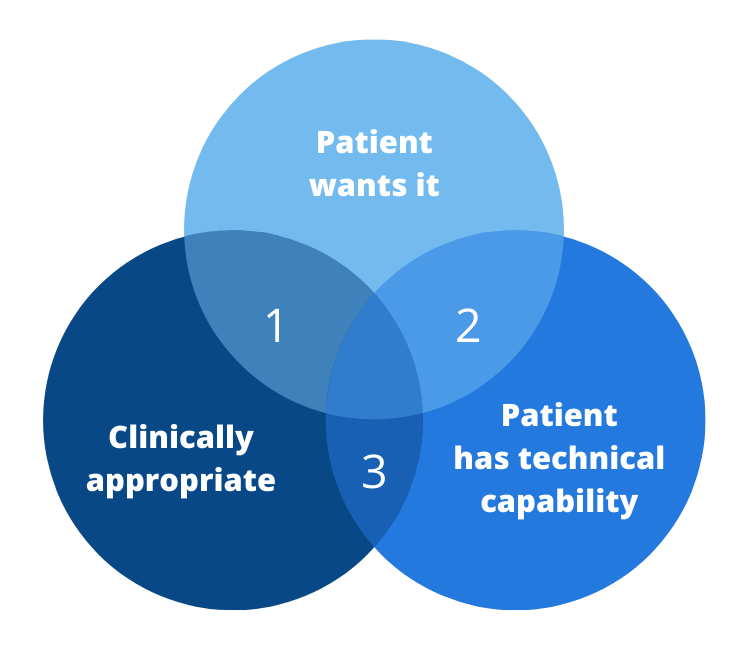
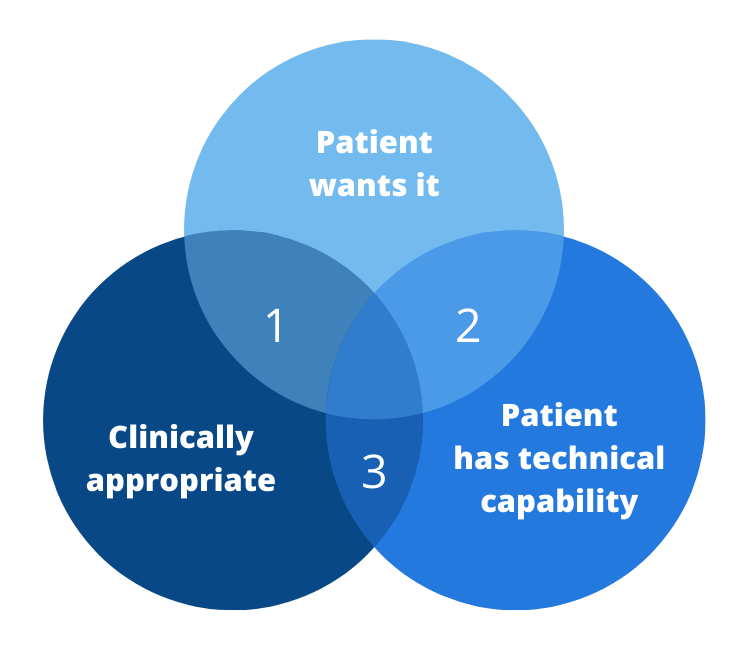
100% Telehealth — Using Telehealth when all criteria are met:
- The patient desires, prefers or is open to telehealth.
- The patient has the technical capabilities.
- Telehealth is clinically appropriate.
Customer Service First: First off, healthcare, as an industry, has an increasing mandate to cater to the desires and the wants of the “modern healthcare consumer”. Gone are the days where the local clinic was the only choice. Nowadays, patients have options – whether it’s urgent care, convenience clinics or online care options. The monopoly of traditional healthcare has been dismantled. Thus if patients desire accessing their care virtually, healthcare organizations that want to stay in business must offer those services to patients.
It’s All or Nothing
For telehealth to be an effective alternative to in-person care, all three of the criteria above must be met.
If only two of the three are met, the results are highly unsatisfactory, as the diagram shows.
We all know from the experience in 2020 and even now what that experience is like: Frustration. When the connectivity causes the video to break down, when hours of technical troubleshooting on how to connect the Bluetooth blood pressure cuff to the remote monitoring hub yield no results, then we know that telehealth is not the right solution.
In this case, using telehealth in this case could be considered as Malpractice – not in the legal sense, but more like an ineffective approach to diagnosis or treatment which ultimately will have to result in an in-person visit.
Three Key Changes to Get to 100%
Rather, I’m encouraging healthcare leaders to approach this opportunity from three different angles that are present quite a shift from the “traditional” approaches and attitudes of the past.
1. Focus on customer service
Secondly, and this is often a bigger stretch, healthcare organizations have to get involved in setting patients up for “technical success”. That means getting involved in improving digital literacy, advocating for better connectivity and preparing patients for telehealth, e.g., through a pre-visit Telehealth TechCheck℠.
2. Define Your Own Clinical Guidelines
We work with our clients to facilitate a process for the clinicians to discuss among themselves to identify what the appropriate standard of care (delivery) should be under various circumstances. When is telephonic care appropriate? When do we need video? Which remote exam tools should we be integrating? When is in-person care the strongly desired choice?
3. Declare, Educate and Train
It’s all about Outcomes








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.





[…] 100% Telehealth is not a Dream […]